KNOW YOUR BODY
DISCUSS YOUR OPTIONS
Now that you know your real risk factors, it's time to take action. Your screening should be based on your unique combination of risk factors. The following section explains what options you may have depending on your risk factors. It is important to remember that none of these screening options should replace a mammogram.
You should always discuss your options with your doctor. If you feel your doctor’s advice or approach is not right for you, you have the right to seek a second (or a third) opinion.
SCREENING MAMMOGRAM
A screening mammogram is an X-ray of the breast; breast imaging radiologists read this X-ray to look for signs of breast cancer. It is a tool that helps women with no known problems or symptoms identify breast cancer at an early stage—when it is most curable.
Mammograms are the most effective screening tool for women who have no other risk factors for breast cancer. In fact, the accuracy rate for mammograms in women without other risk factors is about 84 percent—meaning that mammograms correctly identify breast cancer in about 84 percent of women who actually have the disease. Mammograms are more accurate in women over the age of 50.
How much does it cost?
Medicaid, Medicare, and nearly all insurance companies cover the entire cost of almost all screening mammograms for women age 40 and over. In September 2010, the Affordable Care Act (ACA) required that annual screening mammograms for women over the age of 40 be covered with no copay or deductible.
Even if a woman does not have insurance, she can usually get a free screening mammogram through programs such as the National Breast and Cervical Cancer Control Program, some chapters of the YWCA, and affiliates of The Susan G. Komen Breast Cancer Foundation.
DIAGNOSTIC MAMMOGRAM
Diagnostic mammograms are used as a screening tool for women with signs or symptoms of breast cancer. Diagnostic mammograms are performed the same way as screening mammograms and they are read by the same radiologists.
Diagnostic mammograms differ from screening mammograms in that diagnostic mammograms produce more images of the breast. Otherwise, they are functionally and procedurally the same.
How much does it cost?
With an average cost of about $290, diagnostic mammograms cost more than screening mammograms. Unlike with screening mammograms, not all health insurance programs entirely cover the costs of a diagnostic mammogram.
What if I can't afford it?
The Brem Foundation’s B-Fund will cover the cost of a diagnostic mammogram for any woman who cannot afford it, whose insurance does not cover it, and who cannot have her diagnostic mammogram paid for through another program.
ULTRASOUND
Mammography is an excellent screening tool for breast cancer, but it is not as effective in detecting breast cancers in women with dense breast tissue as it is in women with fatty breast tissue.
In women with dense breasts, mammograms alone miss approximately one-third of breast cancers. However, breast cancer detection in women with dense breasts improves by over 55 percent when mammography and ultrasound are used together. This is because a screening breast ultrasound can detect small, potentially curable cancers that cannot be found on a screening mammogram.
Automated Breast Ultrasound (ABUS) is the first and only ultrasound system developed and FDA-approved for breast cancer screening for women with dense breasts who have not had earlier breast biopsies or surgeries.
How much does it cost?
Unlike screening mammograms, most insurance plans do not cover a breast screening ultrasound. The typical out-of-pocket cost for a breast screening ultrasound is about $250.
Who should consider a screening ultrasound?
If you have dense breast tissue and you do not have other high-risk factors, you should consider ultrasound as an additional screening option. Ultrasound is also a good option for you if you are at high risk and cannot have an MRI.
TOMOSYNTHESIS (3-D MAMMOGRAM)
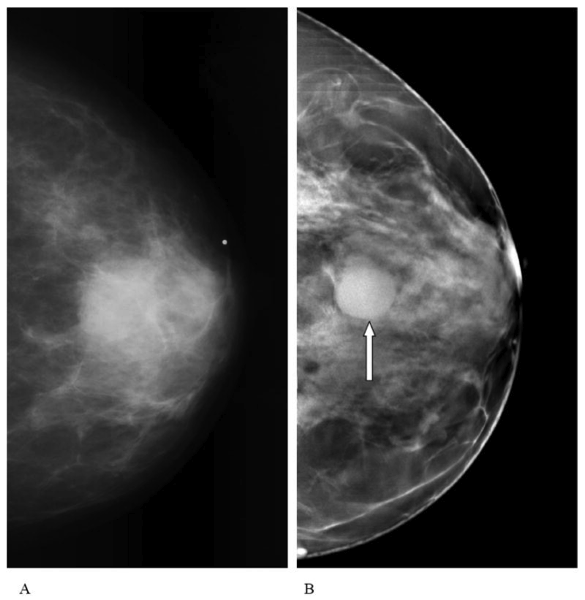
Digital tomosynthesis, also known as 3-D mammography, uses x-rays to create a three dimensional picture of the breast. Tomosynthesis has been shown to significantly increase detection of invasive cancers and decrease recall rates. In addition to finding more cancers, tomosynthesis is more comfortable and uses less radiation than traditional, 2-D mammograms.
Tomosynthesis works by taking multiple images of the breast. These images create a multi-layered 3-D image that exposes cancers previously camouflaged in traditional mammograms. In addition to improving image-quality and cancer detection, tomosynthesis places less pressure on the breast than a traditional mammogram. This alleviates a significant amount of the discomfort sometimes associated with mammograms.
This image from the National Center for Biotechnology Information shows the difference between an image taken with a traditional mammogram (left) and an image taken with tomosynthesis (right).
Who should have tomosynthesis?
Almost all patients are eligible for tomosynthesis. It is especially encouraged for women who have dense breast tissue or prior biopsies or surgery. However it is not available in all healthcare facilities.
How much does it cost?
As of January 1st, 2015, Medicare (and Medicaid in some states) will cover payment for tomosynthesis as long as it is performed in conjunction with 2D digital screening. If a woman’s insurance does not cover the test, the estimated out-of-pocket cost is about $50.
MAGNETIC RESONANCE IMAGING (MRI)
An MRI is an excellent screening tool for you if you are at high risk for getting breast cancer, usually because of a strong family history and/or genetic mutations.
However, be advised that an MRI is not a perfect tool, and not everyone can have an MRI. Therefore, it must be used with mammography in higher-risk women.
Who should get an MRI?
If your risk of getting breast cancer in your lifetime is greater than 20 percent, you should have an MRI every year, usually beginning at age 30. If your risk of getting breast cancer in your lifetime is between 15 and 20 percent, you should discuss an MRI with your doctor.
How much does it cost?
An MRI is more expensive than a mammogram or an ultrasound; the average cost is about $1,084. Some insurance plans will cover screening MRIs if you can prove that you are at high risk for developing breast cancer.
MOLECULAR BREAST IMAGING (MBI)
MBI may be a good screening option for you if you have dense breasts and other risk factors. MBI uses a radioactive tracer that “lights up” areas of cancer in the breast. These areas light up because breast cancer cells absorb more of the radioactive substance than normal cells.
MBI is conducted by injecting a radioactive substance into the patient’s arm. After the substance is injected, a nuclear medicine scanner identifies areas where the radioactive substance is concentrated to show where there may be cancer.
Who should get an MBI?
If you have dense breasts and have other risk factors, MBI may be a good screening option for you.
How much does it cost?
MBI is less expensive than MRI. Some insurance plans cover it but it is not universally covered.
BREAST SELF-EXAMS (BSE)
BSEs are a free, fast, and painless way of screening for breast cancer. BSEs can be done anywhere by anyone, and can be a critical tool in finding early breast cancers when they are most curable. Although some controversy has arisen over the value of BSEs, the Brem Foundation strongly encourages women to do them monthly.
BSEs can help detect early breast cancers—especially when combined with clinical breast exams and annual mammograms.
In fact, about 20 percent of all breast cancers are found through a physical exam rather than though imaging.
When should I do my BSE?
You should do your BSE several days after your period, when your breasts are less tender and swollen. If you are no longer having periods, pick a day that is easy to remember and do it on that day every month.
Where and how should I do my BSE?
In the shower
Use your fingertips to move around your breasts in a circular pattern. You should work from the outside of the breast to the center, being sure to include the armpit area.
Check both breasts every month for any lump, hardening, or thickening. It is important to remember that healthy breasts have different “patterns” and “lumps and bumps.” Doing a BSE every month will help you recognize what is normal for you and what is a change. If you feel something abnormal, call your doctor immediately.
In front of a mirror
Start with your hands at your sides and visually inspect your breasts. Then raise your hands high over your head and visually inspect your breasts. Look for any changes, swelling, or dimpling of the skin, as well as for changes in the nipple.
Lying down
When you lie down, your breast tissue spreads out more evenly along your chest wall.
Put a pillow under your right shoulder and raise your right arm above your head. Use the fingertips of your left hand to make small, circular motions on your right breast using light, medium, and firm pressure. Squeeze the nipple area to check for discharge and lumps. Be sure to inspect your whole breast and armpit area.
Repeat these steps as you inspect your left breast with your right hand.
Early detection saves lives—so know your screening options and risk factors, get screened regularly, and tell every woman you know to do the same!
Quality Care Saves Lives
Breast care alone is not enough. Breast cancer outcomes are correlated with access to excellent care - not any care. In addition to personalized and regular screenings, the quality of breast care that women receive makes a difference in survival rates.
The Brem Foundation strongly encourages women to seek screenings and diagnostic tests from a breast imaging center that is certified as a Breast Imaging Center of Excellence.
Breast Imaging Centers of Excellence (BICOEs) earn accreditation through the American College of Radiology’s Mammography Accreditation Program. A facility with this logo has been designated as an ACR Breast Imaging Center of Excellence by achieving accreditation in all breast imaging modalities. Click here for a full list of Breast Imaging Centers of Excellence and to find a BICOE near you.